Peripheral Artery Disease
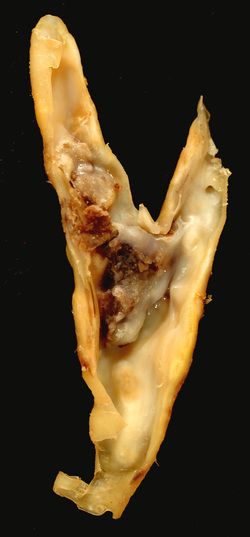
Peripheral arterial disease (PAD) commonly referred to as poor circulation is a condition in which there is restriction of blood flow to the arteries of the extremities such as the legs and feet. Arteries can become restricted due to narrowing of the pathway for blood to travel. This can occur through plaque (the accumulation of cholesterol and other debris), scar tissue, clotting, trauma, or inflammatory response. The narrowing of the vessel pathway prevents oxygen-rich blood from being transported to the extremities.
Symptoms of early peripheral artery disease may be absent. Common symptoms of peripheral arterial disease would include cramping that occurs with activity (intermittent claudication), cramping that occurs while lying down or with the elevation of legs (rest pain), numbness, weakness, cold legs or feet, sores with delayed or lack of healing, loss of hair, change in color/pallor of the skin.
The presence of one or more of the symptoms increases your chances of limb-threatening disease. Also increased is the likelihood of widespread vascular disease which can cause heart attacks and/or strokes.
Risk factors for peripheral vascular disease would include: sedentary lifestyle or lack of exercise, family history, high cholesterol and/or blood pressure, diabetes, smoking, age greater than 50 years old.
If one or more of the symptoms listed above are present it is strongly recommended that you be evaluated by a foot and ankle surgeon or your health care provider. After a thorough history and physical examination which would include: dermatological evaluation, musculoskeletal examination, vascular examination i.e. checking peripheral pulses and vascular testing including one or more of the following: Doppler, duplex ultrasound, ankle brachial test/ index (ABI).
An ankle brachial index is a simple way to obtain a lot of information in regards to vascular disease and the specific location of blockage (if applicable) . This is performed by placing a blood pressure cuff around the arm (of appropriate size) to determine your regular blood pressure ( brachial blood pressure). This is then compared to the lower extremities - most commonly at the ankle but can include the thigh, upper and lower calf, ankle, and toes. By taking your ankle blood pressure of each leg and dividing it by your upper extremity (=brachial) blood pressure (assuming that this is normal) this provides your Doctor with a ratio or percentage. Based off of the ratio, severity of findings can be assessed.
Nonsurgical treatment of peripheral artery disease would include: lifestyle changes such as smoking cessation, exercise, a low-cholesterol/sodium diet, and if applicable monitoring your blood sugar levels. Medication may also be beneficial to prevent blood clots, control blood pressure and cholesterol, and if applicable blood glucose levels.
Depending on the symptoms, findings, and severity surgical intervention may be necessary to allow increased width/vessel diameter or by-passing the blockage . A referral to an appropriate vascular surgeon would be performed if this was necessary as a team approach provides for the most comprehensive care in both the short and long-term.
In order to avoid complications associated with peripheral vascular disease /peripheral arterial disease it is important to follow some simple instructions:
Check your feet on a daily basis. Use of a non glass mirror on the floor may the helpful . If you have difficulty seeing your feet have a friend or family member help with this .
Symptoms of early peripheral artery disease may be absent. Common symptoms of peripheral arterial disease would include cramping that occurs with activity (intermittent claudication), cramping that occurs while lying down or with the elevation of legs (rest pain), numbness, weakness, cold legs or feet, sores with delayed or lack of healing, loss of hair, change in color/pallor of the skin.
The presence of one or more of the symptoms increases your chances of limb-threatening disease. Also increased is the likelihood of widespread vascular disease which can cause heart attacks and/or strokes.
Risk factors for peripheral vascular disease would include: sedentary lifestyle or lack of exercise, family history, high cholesterol and/or blood pressure, diabetes, smoking, age greater than 50 years old.
If one or more of the symptoms listed above are present it is strongly recommended that you be evaluated by a foot and ankle surgeon or your health care provider. After a thorough history and physical examination which would include: dermatological evaluation, musculoskeletal examination, vascular examination i.e. checking peripheral pulses and vascular testing including one or more of the following: Doppler, duplex ultrasound, ankle brachial test/ index (ABI).
An ankle brachial index is a simple way to obtain a lot of information in regards to vascular disease and the specific location of blockage (if applicable) . This is performed by placing a blood pressure cuff around the arm (of appropriate size) to determine your regular blood pressure ( brachial blood pressure). This is then compared to the lower extremities - most commonly at the ankle but can include the thigh, upper and lower calf, ankle, and toes. By taking your ankle blood pressure of each leg and dividing it by your upper extremity (=brachial) blood pressure (assuming that this is normal) this provides your Doctor with a ratio or percentage. Based off of the ratio, severity of findings can be assessed.
Nonsurgical treatment of peripheral artery disease would include: lifestyle changes such as smoking cessation, exercise, a low-cholesterol/sodium diet, and if applicable monitoring your blood sugar levels. Medication may also be beneficial to prevent blood clots, control blood pressure and cholesterol, and if applicable blood glucose levels.
Depending on the symptoms, findings, and severity surgical intervention may be necessary to allow increased width/vessel diameter or by-passing the blockage . A referral to an appropriate vascular surgeon would be performed if this was necessary as a team approach provides for the most comprehensive care in both the short and long-term.
In order to avoid complications associated with peripheral vascular disease /peripheral arterial disease it is important to follow some simple instructions:
Check your feet on a daily basis. Use of a non glass mirror on the floor may the helpful . If you have difficulty seeing your feet have a friend or family member help with this .
- Wear appropriate shoes and socks that fit well and are comfortable.
- When breaking in shoes do this over a long period of time with initial shorter duration.
- Blisters or redness are a sign of irritation and are warning you of potential complications.
- Apply lotions or cream to skin that is excessively dry with use of socks and closed toed Shoegear . For excessive perspiration consider drying agents such as baby powder. If a wound becomes present call your foot and ankle surgeon immediately .
- Do not try to take care of cuts, sores, ingrown toenails or infections by yourself as these usually lead to a worsening of symptoms and possibly limb threatening infections.
- Wash your feet daily. Use warm (not hot) water and a mild soap. Dry your feet—including between the toes—gently and well.
- Keep the skin soft. For dry skin, apply a thin coat of lotion that does not contain alcohol. Apply over the top and bottom of your feet, but not between the toes.
- Trim toenails straight across and file the edges. Keep edges rounded to avoid ingrown toenails, which can cause infections.
- Always wear shoes and socks. To avoid cuts and abrasions, never go barefoot—even indoors.
- Choose the right shoes and socks. When buying new shoes, have an expert make sure they fit well. At first, wear them just for a few hours daily to help prevent blisters and examine the feet afterward to check for areas of irritation. Wear seamless socks to avoid getting sores.
- Check your feet—every day. Check all over for sores, cuts, bruises, breaks in the skin, rashes, corns, calluses, blisters, red spots, swelling, ingrown toenails, toenail infections, or pain.
- Call your foot and ankle surgeon. If you develop any of the above problems, seek professional help immediately. Do not try to take care of cuts, sores, or infections yourself.